Starting the conversation about advance care planning is an important first step in ensuring a person's preferences for future care are known and respected.
If a person's preferences are not known, doctors may use aggressive treatments that the person might not have wanted - and families may feel burdened by the worry that they will make a wrong choice.
Thinking about and planning for the future is a normal part of life so you shouldn't be afraid to raise the subject.
For yourself
You might want to discuss your own plan with your family, friends or carer.
For these conversations, choose a quiet setting where you have a lot of time, so you know that you won’t be interrupted. Be patient and take your time. You don’t need to talk about everything all at once and remember that advance care planning is an ongoing conversation.
Or perhaps you want to talk to friends and family about their own healthcare preferences and plans, especially if they are diagnosed with a serious illness or getting older.
You might also like to talk to your doctor.
The conversation starters below can help you start thinking about what’s important to you.
For family, friends and carers
Serious illness or injury can mean that a person cannot make their own decisions about health care and treatment. Starting planning early helps give the person, their family and their carer peace of mind.
Advance care planning is a normal part of life and is voluntary. Talking about values, beliefs and health and care preferences is an important part of family relationships and friendships. Most people are not used to talking about a time when they can’t make their own decisions, so they may need some time to think before they talk about their choices.
Encourage the person to speak with their family, friends, carer and doctor if they haven’t already.
Advance care planning is an ongoing conversation - it should not happen only one time. Everyone’s values and goals change, what they consider acceptable outcomes might change, so they might want to update their plan.
See the conversation starters below for guidance on starting the conversation.
For health and care workers
Advance care planning conversations should be seen as a normal part of life and of a person’s ongoing healthcare plan. These conversations are voluntary. Encourage people to think about their beliefs, values and preferences regarding their current and future health care. Discuss their attitudes, life goals, and acceptable outcomes regarding healthcare treatment options.
Ideally, advance care conversations should begin when a person is medically stable, comfortable and accompanied by their substitute decision-maker(s), family, friends and/or carer.
Beginning points for advance care planning conversations can include:
- when a person or family member asks about current or future treatment options and goals
- at an age- or condition-related health assessment
- when an older person receives their annual flu vaccination
- when there is a diagnosis of a metastatic malignancy or end organ failure, indicating a poor prognosis
- when there is a diagnosis of early dementia or a disease which could result in loss of capacity
- if you would not be surprised if the person died within twelve months
- if there are changes in care arrangements (for instance, admission to a residential aged care facility).
Care worker conversations
Care workers play an important role in supporting the person with daily activities and listening to their concerns. During your time together you can have conversations about their values and preferences. Also, encourage the person to speak with their family, friends and doctor.
For general practitioners
Consider advance care planning conversations if the patient:
- has an advanced chronic illness (e.g. COPD, heart failure)
- has a life limiting illness (e.g. dementia or advanced cancer)
- is aged 75 years or older, or 55 years or older if they are an Aboriginal and/or Torres Strait Islander person
- is a resident of, or is about to enter, an aged care facility
- is at risk of losing competence (e.g. has early dementia)
- has a new significant diagnosis (e.g. metastatic disease, transient ischemic attack)
- is at a key point in their illness trajectory (e.g. recent or repeated hospitalisation, commenced on home oxygen)
- does not have anyone (e.g. family, caregiver, friend) who could act as substitute decision-maker
- may anticipate decision-making conflict about their future health care
- has a carer
- may likely pass away in the next 12 months.
Language to help raise topics
Health and care professionals, particularly doctors, may find some of the language prompts below helpful when having the conversation
Introducing the topic - ‘I try to talk to all my patients about what they would want if they became more unwell. Have you ever thought about this?’
Speaking for the person - ‘Who would you like me to talk to if you were unable to talk to me about important medical treatment decisions?’
Goals and values - ‘What does it mean to you to ‘live well’? What are your goals at this time?’
Care and treatment - ‘What do you understand about where things stand right now with your illness?’
Concluding the conversation - ‘Thank you for clarifying your goals, values and acceptable outcomes. Does your family (or carer or friends) know what you would want?’
Training and education
Learn more about starting the conversation about advance care planning through our training and education.
Conversation starters
Here are a few suggestions about how everyone can start the conversation about advance care planning.
Health and care workers may find it helpful to show this to patients when talking about their planning.
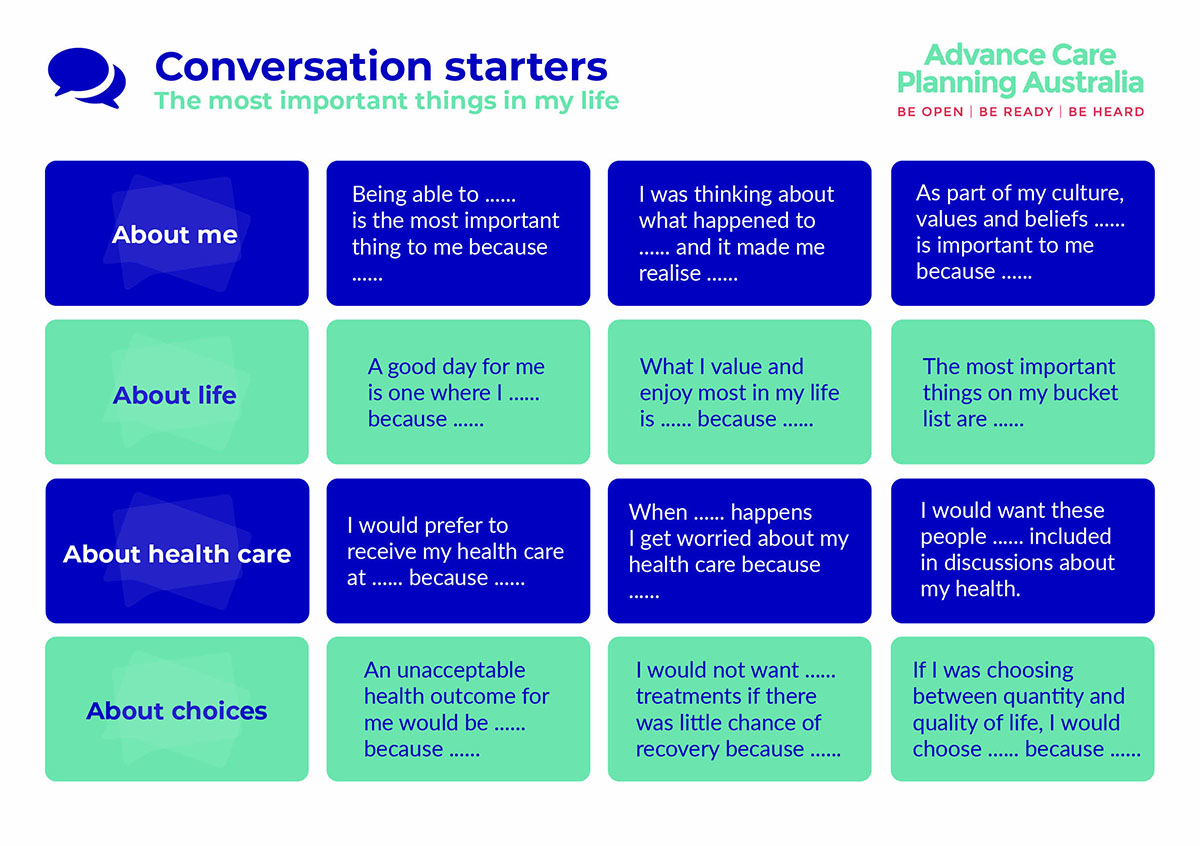
Printable version [PDF 521.67 KB]
Get support
Contact our National Advance Care Planning Support ServiceTM on 1300 208 582 for more guidance on starting the conversation. We're available 9am – 5pm, Monday – Friday (AEST).
See also
- Introduce advance care planning as part of routine care (video for health professionals).