
Tasmania Conference in Hobart by our Education Manager, Rebecca Taylor.
Rebecca presented ‘How advance care planning informs quality of life for people over 85 years’, which was prepared by our Program Director, Xanthe Sansome. The presentation included information from statements made on older people’s advance care planning documents that were used as part of Xanthe’s Masters Research Thesis when she worked with Queensland’s Office of Advance Care Planning.
This research showed that 82% of people over 85 years with a completed advance care planning document did not want CPR and 85% did not want life prolonging treatments. These preferences were more likely in females, those who lived in residential care facilities and who had lost decision-making capacity, with increasing age being the dominant factor in these factors. The more telling information, however, was in the comments about what they valued or enjoyed most in life, what was unacceptable and what they would like considered as they neared their end of life.
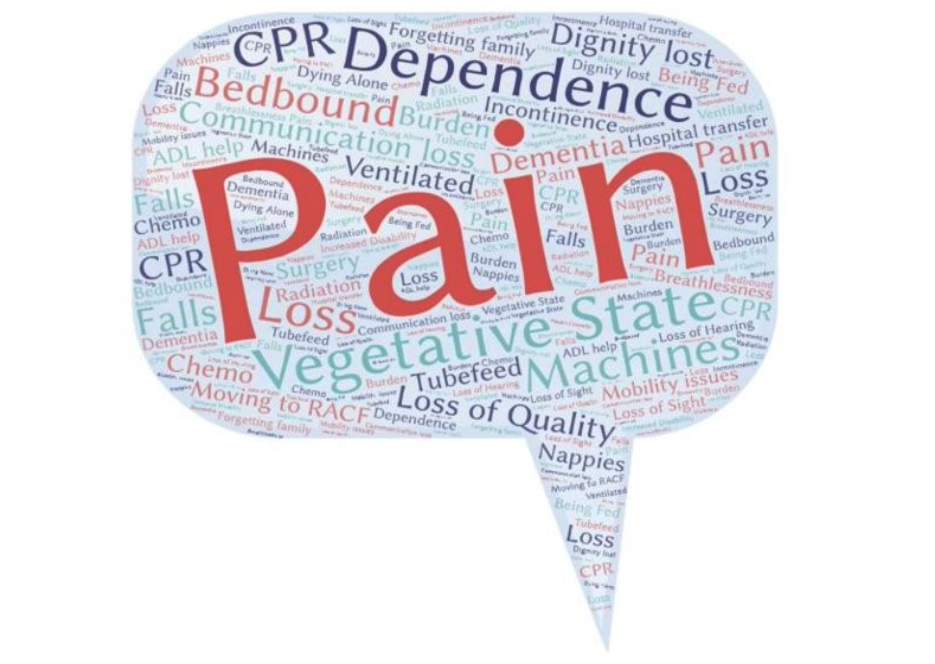
The following word pictures capture some of the themes from older people’s Statement of Choices documents.
What they value or enjoy most in life

What would be unacceptable situations
What people would like when they are nearing death

Rebecca’s presentation also captured how people she cared for as a registered nurse in ICU, advance care planning and palliative care in aged care have shaped her knowledge of ACP. Throughout Rebecca’s clinical experience, it was repeatedly highlighted how having advance care planning conversations or, more particularly, a document, made a huge difference to the dying person, their family and professionals providing care.
Rebecca explained, “Considering a person’s values - and what quality of life does and does not look like for them - can help guide advance care planning conversations and provide the right care. It’s really helpful to know ahead of time what a person wants for quality of life as well as their preferences for CPR or hospital transfers. To have discussed these things openly with the person, their family and other members of the health care team, means all involved in the end of this person’s life are ‘on the same page’. When deterioration occurs, discussions can occur with more calm and empathy, with acknowledgement of the dying person’s wishes.
“To be able to provide aspects of care that are so important to a person brings great personal satisfaction. These aspects of care may include the presence of family, religious leader or favourite music or pet. Or it may include the absence of pain, suffering, or transfers to hospital. Knowing these important aspects of care enables staff and family to focus on the dying person’s immediate needs. It doesn’t take away the sadness of the loss but means people who have loved or cared for the person know they have done their best for them, right up to their final breath.”